Spatially fractionated radiotherapy is a novel cancer treatment that uses a pattern of alternating high-dose peaks and low-dose valleys to deliver a nonuniform dose distribution. Numerous preclinical investigations have demonstrated that by shrinking the peaks and valleys to submillimetre dimensions, the resulting microbeams confer extreme normal tissue tolerance, enabling delivery of extremely high peak doses and providing excellent tumour control.
The technique has not yet, however, been used to treat patients. Most preclinical studies employed synchrotron X-ray sources, which deliver microbeams at ultrahigh dose rates but are not widely accessible. Another obstacle is that these extremely narrow beams (100 µm or less) are highly sensitive to any motion during irradiation, which can blur the pattern of peak and valley doses.
Instead, a team at the Mayo Clinic in Rochester, Minnesota, is investigating the clinical potential of minibeam radiation therapy (MBRT), which employs slightly wider beams (500 µm or more) spaced by more than 1000 µm. Such minibeams still provide high normal tissue sparing and tumour control, but their larger size and spacing makes them less sensitive to motion. Importantly, minibeams can also be generated by conventional X-ray sources with lower dose rates.
Michael Grams and colleagues have now performed the first patient treatments using MBRT. Writing in the International Journal of Radiation Oncology, Biology, Physics, they describe the commissioning of a clinical radiotherapy system for MBRT and report on the first two patients treated.
Minibeam delivery
To perform MBRT, the researchers adapted the Xstrahl 300, a clinical orthovoltage unit with 180 kVp output. “Because minibeam radiotherapy uses very narrow beams of radiation spaced very closely together, it requires low-energy orthovoltage X-rays,” Grams explains. “Higher-energy X-rays from linear accelerators would scatter too much and blur the peaks and valleys together.”
The team used cones with diameters between 3 and 10 cm to define the field size and create homogeneous circular fields. This output was then split into minibeams using tungsten collimators with 0.5 mm wide slits spaced 1.1 mm apart.
Commissioning measurements showed that the percentage depth dose decreased gradually with depth, reaching 50% somewhere between 3.5 and 4 cm. Peak-to-valley ratios were highest at the surface and inversely related to cone size. Peak dose rates at 1 cm depth ranged from 110 to 120 cGy/min.
The low dose rate of the orthovoltage system means that treatment times can be quite long and patient motion may be an issue. To mitigate motion effects, the researchers created 3D printed collimator holders that conform to the patient’s anatomy. These holders are fixed to the patient, such that any motion causes the patient and collimator to move together, maintaining the spatial separation of the peak and valley doses.
“This treatment had never been delivered to a human before, so we had to figure out all of the necessary steps in order to do it safely and effectively,” says Grams. “The main challenge is patient motion, which we solved by attaching the collimator directly to the patient.”
First-in-human treatments
The team treated two patients with MBRT. The first had a large (14x14x11 cm) axillary tumour that was causing severe pain and restricted arm motion, prompting the decision to use MBRT to shrink the tumour and preserve normal tissue tolerance for future treatments. He was also most comfortable sitting up, a treatment position that’s only possible using the orthovoltage unit.
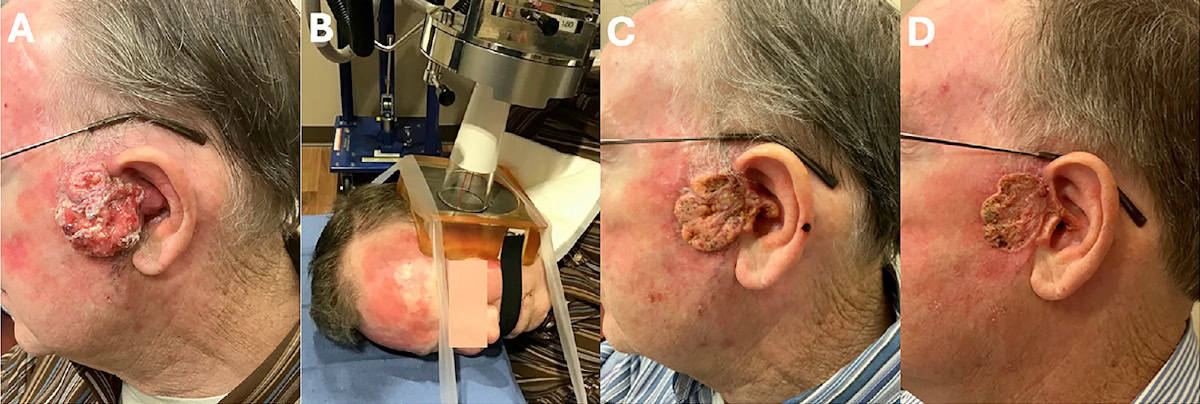
The second patient had a 7x6x3 cm ear tumour that completely blocked his external auditory canal, causing hearing loss, shooting pain and bleeding. He was unable to undergo surgery due to a fear of general anaesthesia and instead was recommended MBRT to urgently reduce pain and bleeding without compromising future therapies.
“These patients had very few treatment options that the attending physician felt would actually help mitigate their symptoms,” explains Grams. “Based on what we learned from our preclinical research, they were felt to be good candidates for MBRT.”
Both patients received two daily MBRT fractions with a peak dose of 1500 cGy at 1 cm depth, using the 10 cm cone for patient 1 and the 5 cm cone for patient 2. The radiation delivery time was 11.5 or 12 min per fraction, with the second fraction delivered after rotating the collimator by 90°.
Prior to treatment, the collimator was attached to the patient and a small piece of Gafchromic film was placed directly on the tumour for in vivo dosimetry. For both patients, the films confirmed the pattern of peak and valley doses, with no evidence of dose blurring.
For patient 1, the measured peak and valley doses were 1900 and 230 cGy, respectively. The expected doses (based on commissioning measurements) were 2017 and 258 cGy, respectively. Patient 2 had measured peak and valley doses of 1800 and 180 cGy, compared with expected values of 1938 and 248 cGy.
Both patients exhibited positive clinical responses to MBRT. Six days after his second treatment, patient 1 reported resolution of pain and improved arm motion. Three weeks later, the tumour continued to shrink and his full range of motion was restored. Despite the 10 cm cone not fully encompassing the large tumour, a uniform decrease in volume was still observed.
After one treatment, patient 2 had much reduced fluid leakage, and six days later, his pain and bleeding had completely abated and his hearing improved. At 34 days after MBRT, he continued to be asymptomatic and the lesion had completely flattened. Pleased with the outcome, the patient was willing to reconsider the recommended standard-of-care resection.
“The next step is a formal phase 1 trial to determine the maximum tolerated dose of minibeam radiotherapy,” Grams tells Physics World. “We are also continuing our preclinical work aimed at combinations of MBRT and systemic therapies like immunotherapy and chemotherapy drugs.”
The post First patients treated using minibeam radiation therapy appeared first on Physics World.

